
4 Reasons Why Your Patient’s LPR Symptoms Didn’t Improve Despite PPI Therapy
January 30, 2018“Early Referral for Esophageal pH Monitoring is More Cost-Effective than Prolonged Empiric Trials of PPIs for Suspected Gastroesophageal Reflux Disease”
February 28, 2018By: Craig H. Zalvan, MD, FACS
Chief of Otolaryngology and Medical Director
The Institute for Voice and Swallowing Disorders
CASE HISTORY & EVALUATION
66 year old male presents with diagnosis of GERD and asthma for chronic cough. He reports being well until 5 years ago when he had a severe URI, symptoms of which resolved, except for a chronic cough. Additional symptoms of ongoing waterbrash, throat clearing, and globus sensation; a tickle sensation in the throat followed by spasms of coughing associated with bouts of “wheezing,” described as a high pitch sound when breathing inward. He also reports his eyes tearing, rhinorrhea, and vocal strain with occasional bouts of nausea. Cold air and talking trigger coughing episodes.
Prior treatment included multiple courses of antibiotics, steroids, and allergy medications with no change in symptoms. A GI put him on twice daily PPI therapy that did seem to decrease coughing at night but not during the day. ENT evaluation was reported as normal. Pulmonology evaluation demonstrated normal PFT, yet diagnosis was “cough variant asthma.” Patient was placed on an inhaled steroid and bronchodilator (which at times triggered coughing) with no significant improvement. CT of the sinus, CXR, CT of the chest were all WNL. His initial Reflux Symptom Index, RSI=36; initial Cough Symptom Index, CSI=32.
Evaluation revealed normal sinus anatomy and laryngoscopy demonstrated a slight left vocal paresis, normal upper trachea, and findings consistent with LPR – moderate posterior glottic edema, vocal fold edema, sub-vocal fold edema, and obliteration of the ventricle. Transnasal esophagoscopy demonstrated mild esophagitis with LA Grade A findings.
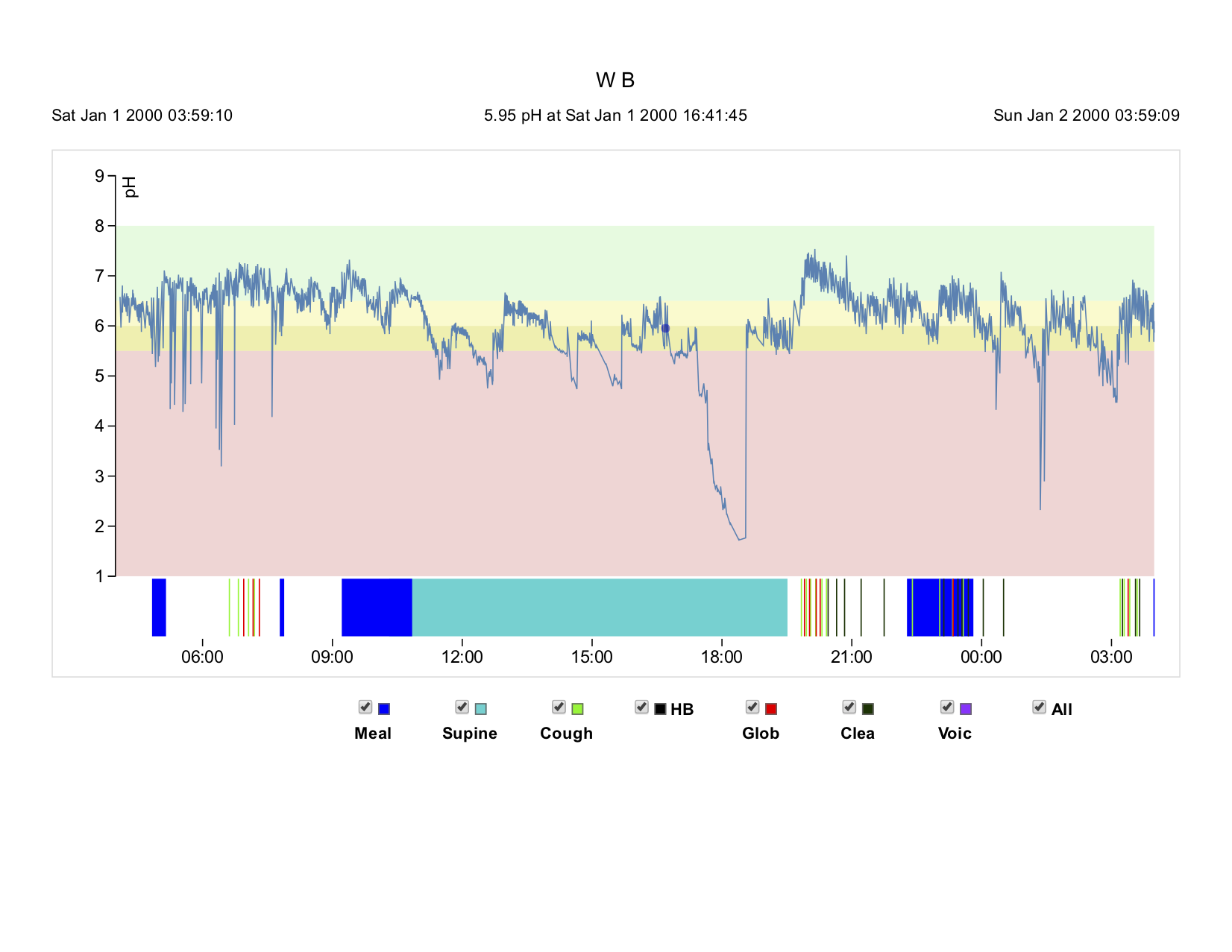
Oropharyngeal pH testing was ordered given the chronicity of his symptoms and lack of response to most medications. Testing was performed while on PPI therapy, as cessation of the medications resulted in significantly increased burning and coughing at night.
DIAGNOSIS
Given the close association with his initial URI, a diagnosis of a post-viral neurogenic chronic cough with post-viral LPR exacerbation causing the night-time coughing and acting as a day-time trigger.
ABOUT LPR
Laryngopharyngeal reflux disease (LPRD) represents a spectrum of symptoms affecting the upper aerodigestive tract, including: throat clearing, globus sensation, dysphagia, waterbrash, hoarseness, and chronic cough. LPR is thought to be caused by exposure of the laryngopharyngeal tissues to acid in the presence of pepsin, with resulting inflammation.
Diagnosis is typically based on history and physical examination with oropharyngeal pH testing utilized for recalcitrant symptoms, confounding factors, and diagnostic dilemmas.
Treatment is controversial and has historically utilized proton pump inhibitors (PPI), despite questionable potential efficacy2 and negative side effects including: increased rates of heart attack, dementia, and overall rates of death for long term use3. Over 13 billion dollars4 are spent yearly in attempt to treat this disease, primarily due to the cost of drug utilization. Recent evidence suggests that a mostly plant based, Mediterranean style diet, with the use of alkaline water, can significantly control this disease as well, if not better, than PPI5.
DISCUSSION
Chronic cough is a diagnostic dilemma resulting in significant expenditure of time, money, and resources. In the otolaryngology world, the causes of chronic cough can be broken down into four main categories: sinus, pulmonary, reflux-related, and intrinsic to the larynx.
Sinus: This patient had prior treatment for sinus disease and had a normal sinus CT. Sinus disease can certainly cause coughing from increased volume of nasal drainage of mucus, allergic mucin, and pus; however, should be associated with other symptoms of headache, fever, facial pain, pressure, sneezing, rhinorrhea, and malaise as well as physical findings on endoscopy demonstrating drainage of thick mucus, pus, inflammatory polyps, and/or bleeding. The addition of CT scanning of the sinus would also demonstrate significant abnormalities suggesting the sinuses as the cause.
The pulmonary workup was completely normal despite being labeled as “cough-variant asthma” and he had no response to multiple inhalers. The addition of a normal CT of the chest, CXR, and PFT sheds significant doubt on the diagnosis of “cough-variant asthma”. Cough variant asthma does exist as a real entity: chronic cough with high sputum eosinophilia, reversible airway disease, and response to inhaled steroids/bronchodilators. Nearly all of the chronic cough patients seen in the laryngology practice for chronic cough do not fit into this criteria. Neurogenic cough is far more common and likely represents the vast majority of cough variant asthma patients6, typically consisting of chronic cough preceded by a tickle sensation followed by coughing spasms often associated with epiphora, rhinorrhea, vocal strain, and nausea. The cough is often triggered by talking, laughing, eating, drinking, cold air, and odors. These spasms of coughing can be accompanied by bouts of inspiratory stridor, often misdiagnosed as “wheezing” further propagating the false diagnosis of asthma. Treatment in our clinic is first based on trigger reduction: saline irrigations and topical steroids/antihistamines to decrease and thin the basal rate of mucus from the sinuses, often upwards of 1L or more.
Reflux-related: LPR represents another potential trigger and our data suggest a dietary approach using a mostly plant based, Mediterranean style diet of fruits, vegetables, grains, and nuts with alkaline water decreases LPR and removes the potential trigger effect. In addition to treating reflux, our diet approach helps protect against diabetes, stroke, heart disease, and many cancers7. Our results* demonstrate upwards of 70% of people experience a more than 50% reduction in coughing using this approach alone, without medications†. Lastly, LPR itself can be a cause of chronic coughing, often with night-time awakening as one of the symptoms and treatment is mostly diet based.
TREATMENT
Trigger reduction therapy was initiated: nasal saline irrigation and nasal antihistamine/steroid combination sprays to decrease and thin the basal rate and consistency of nasal secretions. LPR was treated using a plant based, Mediterranean style diet of 90-95% fruits, vegetables, grains, and nuts; and alkaline water (pH>8.0). Patient’s PPI’s were reduced to a single evening dose. Within 1 week he reported substantial improvement with his daytime coughing and complete cessation of coughing while sleeping. He lost 6 pounds and was instructed to taper off the PPI. By his next visit 6 weeks later, he had lost a total of 10 pounds and his coughing during the day also had improved greatly. His follow-up RSI=8 and his CSI=6 with complete cessation of his PPI.
TAKE HOME POINTS
1. Oropharyngeal pH testing is an important tool in determining the presence of reflux or the absence of reflux.
2. Most patients presenting to the laryngology clinic have seen multiple other physicians and have tried multiple other approaches and medication with failure.
3. Oropharyngeal pH testing can be utilized to demonstrate ongoing LPR despite being on PPI therapy, further underlining the need for major dietary changes. Additionally, oropharyngeal pH testing can demonstrate the absence of reflux supporting the diagnosis of chronic neurogenic cough.
* manuscript in preparation
† Neuromodulating drugs such as amitriptyline can be utilized
REFERENCES
1 Ayazi S, Lipham JC, Hagen JA, et al. A New Technique for Measurement of Pharyngeal pH: Normal Values and Discriminating pH Threshold. J Gastrointest Surg. 2009 Aug;13(8):1422-9.
2 Karkos PD, Wilson JA. Empiric treatment of laryngopharyngeal reflux with proton pump inhibitors: a systematic review. Laryngoscope 2006;116:144-8.
3 Corsonello A, Lattanzio F, Bustacchini S , et al. Adverse events of proton pump inhibitors: potential mechanisms. Curr Drug Metab. 2017 Dec 7. doi:
10.2174/1389200219666171207125351. [Epub ahead of print]
4 Sheen E, Triadafilopoulos G. Adverse effects of long-term proton pump inhibitor therapy. Digest Dis Sci 2011;56:931-50.
5 Zalvan CH, Hu S, Greenberg B, Geliebter J. A Comparison of Alkaline Water and Mediterranean Diet vs Proton Pump Inhibition for Treatment of Laryngopharyn
geal Reflux. JAMA Otolaryngol Head Neck Surg. 2017 Oct 1;143(10):1023-1029. doi: 10.1001/jamaoto.2017.1454.
6 Bastian RW. Diabolical Coughing-Prima Facie Protocols for Diagnosis and Treatment of Medically Jaded Patients. JAMA Otolaryngol Head Neck Surg. 2016 Sep
1;142(9):889-90. doi: 10.1001/jamaoto.2016.0973.
7 Orlich MJ, Singh PN, Sabate J, et al. Vegetarian dietary patterns and mortality in Adventist Health Study 2. JAMA Intern Med 2013;173:1230-8.

