“Quantifying Laryngopharyngeal Reflux in Singers: Perceptual and Objective Findings”
February 28, 2018RESTECH ACQUIRES STRETTA® and SECCA®
April 24, 2018Commonly referred to as “silent reflux,” laryngopharyngeal reflux (LPR) has long been difficult for physicians to diagnose because of its nonspecific symptoms. The traditional approach to assessing LPR symptoms relies on response to empiric treatment and symptom improvement using the reflux symptom index (RSI) or reflux finding score (RFS). Without clear criteria in place, these tools are highly subjective.
 RSI & pH Testing
RSI & pH Testing
The RSI is a nine-item questionnaire administered to patients to document LPR symptoms and severity over the past month. The scoring system uses a scale of 0 (no problem) to 5 (severe), with a maximum total score of 45. A total score of 13 or greater is considered a positive case of LPR.1
The degree of concurrence between symptom severity (as determined by the RSI) and pH findings (as determined by objective testing) is inconsistent. Self-reported symptom scores do not reliably predict presence or severity of acid reflux disease.2
Studies show that there is no significant difference in chronic laryngitis patients in their presenting symptoms, severity, or duration, with or without pharyngeal reflux.2 There was also no significant difference in RSI seen between RYAN+ and RYAN− patients.3 (The RYAN Score was created by Dr. Tom DeMeester with high specificity for severe reflux patients using thresholds of pH 5.5 for upright and pH 5.0 for supine positions.)
Data suggests that over 40% of patients with an RSI <13 will have a positive RYAN score.3
This finding highlights the RSI’s subjective nature and the high possibility of response bias in patient self-assessment questionnaires. Patients with a low RSI may still have severe reflux according to objective pH tests.
Anxiety and Depression
The presence of anxiety and depression impairs the predictive value of the RSI for LPR as patients with psychiatric disorders tend to exaggerate physical symptoms.
In Oyer’s retrospective study, patients in the psychiatric disorder (+PSY) group had a significantly higher RSI on average, but only half the rate of abnormal (LPR +) pH studies as compared to the non-psychiatric (−PSY) group.4 Among −PSY patients alone, the average RSI was significantly higher for patients with an abnormal pH study than for those with a normal pH study.4 These results highlight the effects of psychiatric disorders on patient-perceived symptoms reported on the RSI and indicate that anxiety and depression inflate the RSI, impairing its predictive value for LPR.
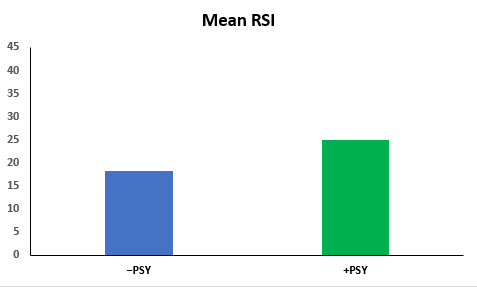
The mean RSI of the psychiatric disorder group was higher than that of the non-psychiatric disorder group. However, the psychiatric disorder group actually had a lower incidence of abnormal pH probe studies.
These findings pose a potential explanation for criticisms of the RSI’s subjective nature. With many outside variables affecting the accuracy of the RSI, including mental health, the diagnostic utility of the RSI in diagnosing LPR is limited.
Read more about evidence-ased pH testing for LPR symptoms.
Would you like to learn more about how Restech pH testing could benefit your practice?
References
- Austin J. Rating Laryngophargyneal Reflux Severity: How Do Two Common Instruments Compare? ENTtoday. 2006 Aug. http://www.enttoday.org/article/rating-laryngopharyngeal-reflux-severity-how-do-two-common-instruments-compare/
- Beaver ME, Karow CM. Clinical Utility of 24 Hour Pharyngeal pH Monitoring for Hoarseness. J Laryngol Voice. 2012;2(2):60-3.
- Friedman M, Hamilton C, Samuelson CG, et al. The Value of Routine pH Monitoring in the Diagnosis and Treatment of Laryngopharyngeal Reflux. Otolaryngol Head Neck Surg. 2012; 146(6):952-8.
- Oyer SL, Anderson LC, Halum SL. Influence of Anxiety and Depression on the Predictive Value of the Reflux Symptom Index. Ann Otol Rhinol Laryngol. 2009;118(10):687-692.

